Early diagnosis is essential for improved patient management and prognosis. Learn about ICCS and other expert recommendations for who should be tested for PNH.
PNH is a chronic, hemolytic disease with risk of unpredictable and life-threatening complications1
- Approximately 20%-35% of patients with PNH (receiving historical supportive care, including oral anticoagulant therapy and transfusions) die within 5-10 years of diagnosis2-5
Learn more about some of these life-threatening complications by clicking on the links below.
Thrombosis is the leading cause of death in PNH, and even the first thrombotic event can be fatal6
64% of patients with PNH have chronic kidney disease (CKD), which in advanced stages is associated with premature mortality7
40% to 67% of deaths are due to venous or arterial thrombosis1,9
- Thromboembolism (TE) in PNH is complex and may occur at any site, including intra-abdominal and cerebral veins8,10
- 35% of patients had multiple TE events10
- 31% of TEs occurred at arterial sites, including cerebral arteries and myocardial infarction10
- Initial TE increases relative risk of death in PNH 5- to 10-fold6
- Patients with PNH with thrombosis at presentation have only a 40% survival rate at 4 years8
- PNH is associated with a highly increased risk of thrombosis11
- Patients with PNH are 62x more likely to have a venous TE (VTE) vs the general population,
and relative risk of VTE is greater in PNH vs other inherited hypercoagulable states11
- Patients with PNH are 62x more likely to have a venous TE (VTE) vs the general population,
- Patients with PNH frequently experience new thrombotic episodes despite anticoagulation10
- In a recent study, 50% of TE occurred while patients were on anticoagulants4
Chronic, complement-mediated hemolysis causes progressive renal damage in patients with PNH7
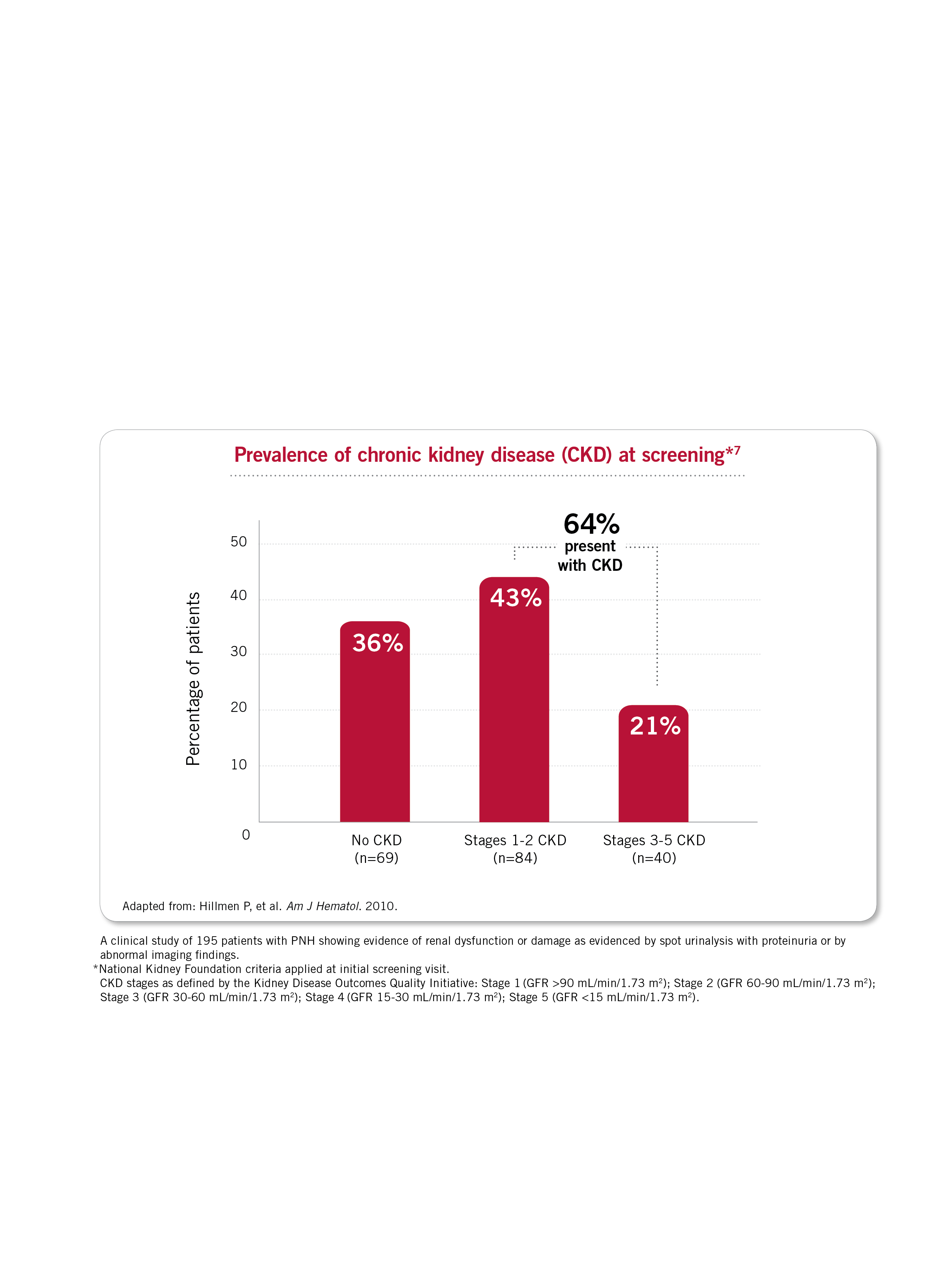
Renal failure is the second leading cause of death in patients with PNH1
- Renal failure accounts for approximately 8% to 18% of patient deaths in PNH1
- Virtually all patients with PNH have evidence of renal damage by biopsy, imaging techniques, or at postmortem examination7
PNH has been called “the most vicious acquired thrombophilic state known in medicine”.8 Learn which common symptoms are associated with an increased risk of thromboembolism in a patient diagnosed with PNH.
References: 1. Hillmen P, et al. Br J Haematol. 2013;162(1):62-73. 2. Peffault de Latour RP, et al. Blood. 2008;112(8):3099-3106. 3. Loschi M, et al. Am J Hematol. 2016;91(4):366-370. 4. Kelly RJ, et al. Blood. 2011;117(25):6786-6792. 5. Hillmen P, et al. N Engl J Med. 1995;333(19):1253-1258. 6. Hillmen P, et al. Blood. 2007;110(12):4123-4128. 7. Hillmen P, et al. Am J Hematol. 2010;85(8):553-559. 8. Hill A, et al. Blood. 2013;121(25):4985-4996. 9. Sharma VR. Clin Adv Hematol Oncol. 2013;11 Suppl 13(9):2-8. 10. Lee JW, et al. Int J Hematol. 2013;97(6):749-757. 11. McKeage K. Drugs. 2011;71(17):2327-2345.

