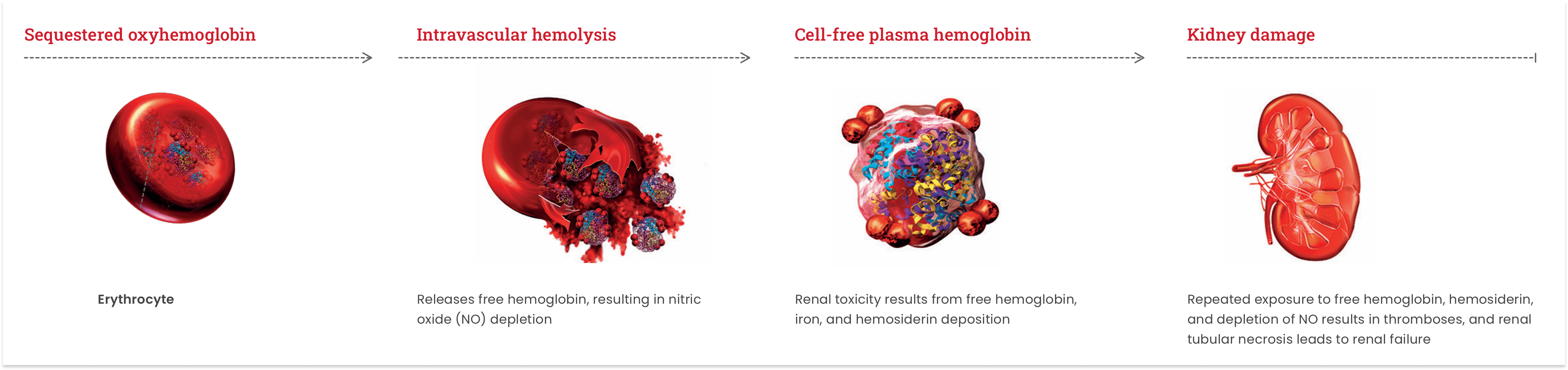
Evidence of renal damage has been shown in nearly all patients with PNH via biopsy, imaging techniques, or postmortem examination3-9
Mortality
Renal failure
is the second leading cause of death in patients with PNH.10,11
Prevalence of chronic kidney disease at screening3,a,b

Mortality
Renal failure
is the second leading cause of death in patients with PNH.10,11
Adapted from: Hillmen P, et al. Am J Hematol. 2010.
aA clinical study of 195 patients with PNH showing evidence of renal dysfunction or damage as evidenced by spot urinalysis with proteinuria or by abnormal imaging findings. CKD stages as defined by the Kidney Disease Outcomes Quality Initiative: Stage 1 (GFR >90 mL/min/1.73 m2); Stage 2 (GFR 60-90 mL/min/1.73 m2); Stage 3 (GFR 30-60 mL/min/1.73 m2); Stage 4 (GFR 15-30 mL/min/1.73 m2); Stage 5 (GFR <15 mL/min/1.73 m2).3
bNational Kidney Foundation criteria applied at initial screening visit.
In PNH, terminal complement–mediated attack on red blood cells leads to free hemoglobin and hemosiderin deposits that contribute to chronic kidney disease in PNH3,12-14
Thrombosis in PNH can be life-threatening and can occur at any site15
Multiple sites may be involved in more than one-fifth of cases.15
Sites of thrombosis in patients with PNH16,c,d
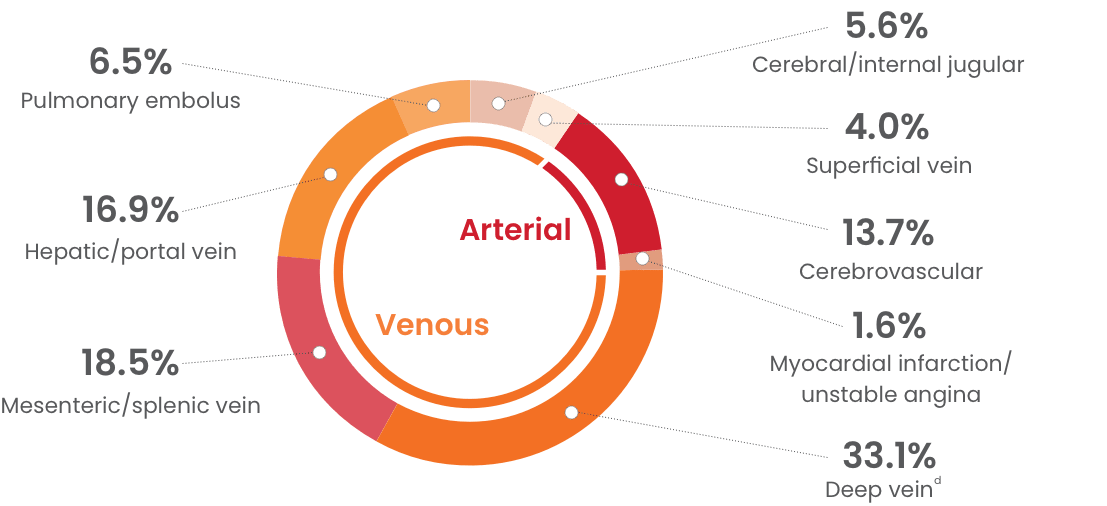
cData pooled from examining the medical histories of patients with PNH (N=195) from 3 independent studies. Thrombotic events occurred in 63 patients: 1 event in 35 patients, 2 events in 15 patients, 3 events in 7 patients, and ≥5 events in 6 patients.16
dIncludes events in lower extremity (n=23) and other locations (n=18; including inferior vena cava, bilateral lower extremity, pelvic, ureter, axillary, subclavian, and brachiocephalic veins).16


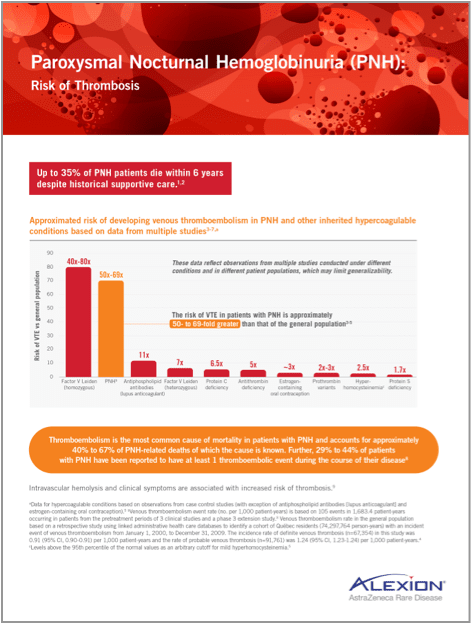
The risk of venous thromboembolism in patients with PNH is high
Approximated risk of developing venous thromboembolism (VTE) in PNH and other inherited hypercoagulable conditions based on data from multiple studies16-20,e
The risk of VTE in patients with PNH is approximately 50- to 69-fold greater than that of the general population16-18


These data reflect observations from multiple studies conducted under different conditions and in different patient populations, which may limit generalizability.
eData for hypercoagulable conditions based on observations from case-control studies (with exception of antiphospholipid antibodies [lupus anticoagulant] and estrogen-containing oral contraception).18
fVenous thromboembolism event rate (no. per 1,000 patient-years) is based on 105 events in 1,683.4 patient-years occurring in patients from the pretreatment periods of 3 clinical studies and a phase 3 extension study.16 Venous thromboembolism rate in the general population based on a retrospective study using linked administrative healthcare databases to identify a cohort of Québec residents (74,297,764 person-years) with an incident event of venous thromboembolism from January 1, 2000, to December 31, 2009. The incidence rate of definite venous thrombosis (n=67,354) in this study was 0.91 (95% CI, 0.90-0.91) per 1,000 patient-years and the rate of probable venous thrombosis (n=91,761) was 1.24 (95% CI, 1.23-1.24) per 1,000 patient-years.17
gLevels above the 95th percentile of the normal values as an arbitrary cutoff for mild hyperhomocysteinemia.18
THROMBOEMBOLISM
~40% to 67% of PNH‑related deaths
Thromboembolism is the most common cause of mortality in patients with PNH and accounts for approximately 40% to 67% of PNH-related deaths of which the cause is known.15
THROMBOEMBOLIC EVENT
29% to 44%
of patients
29% to 44% of patients with PNH have been reported to have at least 1 thromboembolic event during the course of their disease.15
- Sharma VR. Clin Adv Hematol Oncol. 2013;11(9)(suppl 13):2-8.
- Hill A, et al. Nat Rev Dis Primers. 2017;3:17028.
- Hillmen P, et al. Am J Hematol. 2010;85(8):553-559.
- Clark DA, et al. Blood. 1981;57(1):83-89.
- Nguyen JS, et al. N Engl J Med. 2006;355(10):1048-1052.
- Rimola J, et al. Br J Radiol. 2004;77(923):953-956.
- Suzukawa K, et al. Intern Med. 1993;32(9):686-690.
- Tanaka YO, et al. J Comput Assist Tomogr. 1993;17(5):749-753.
- Zachée P, et al. Clin Nephrol. 1993;39(1):28-31.
- Nishimura JI, et al. Medicine (Baltimore). 2004;83(3):193-207.
- Hillmen P, et al. Br J Haematol. 2013;162(1):62-73.
- Kelly R, et al. Ther Clin Risk Manag. 2009;5:911-921.
- Rother RP, et al. JAMA. 2005;293(13):1653-1662.
- Tsai CW, et al. Kidney Int. 2007;71(11):1187.
- Hill A, et al. Blood. 2013;121(25):4985-4996.
- Hillmen P, et al. Blood. 2007;110(12):4123-4128.
- Tagalakis V, et al. Am J Med. 2013;126(9):832.e13-832.e21.
- De Stefano V, et al. Haematologica. 2002;87(10):1095-1108.
- Wahl DG, et al. Lupus. 1998;7(1):15-22.
- Vinogradova Y, et al. BMJ. 2015;350:h2135.