Testing for PNH: Flow cytometry and LDH
PNH diagnosis consists of recognizing the symptoms patients exhibit and testing to confirm PNH diagnosis
High-sensitivity flow cytometrya is the gold standard diagnostic test for PNH1-3
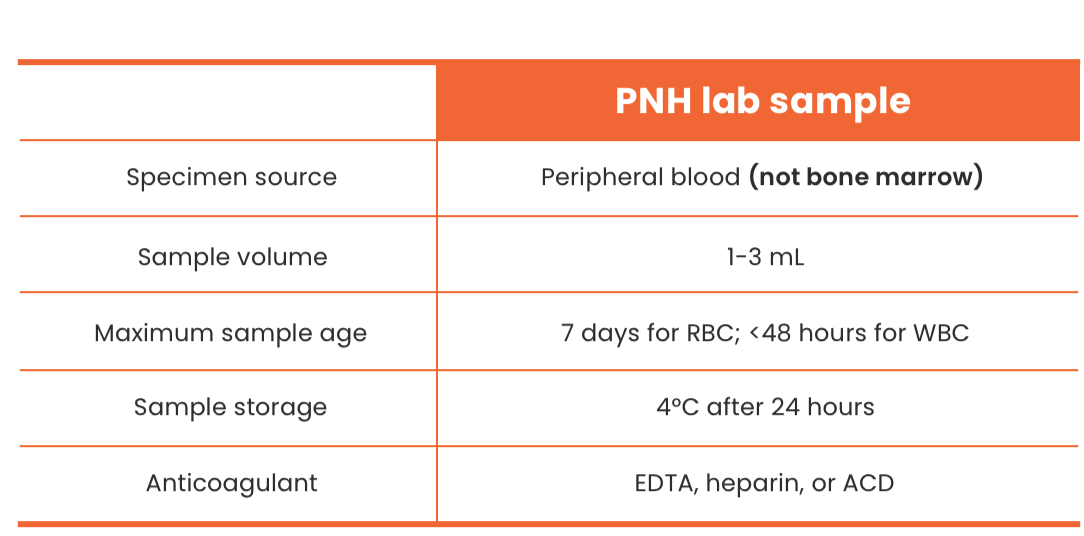
- High-sensitivity flow cytometry (HSFC) is performed on peripheral blood—not bone marrow1,2
- Labs should perform PNH HSFC on white blood cells (WBCs) (using >1 reagent) and on red blood cells (RBCs)1,4
- Granulocytes using FLAER/CD24 or FLAER/CD157 combinations give most accurate estimate of PNH clone size2
- Evaluation of RBCs alone may not be accurate due to hemolysis and the dilution effect of transfusions1,4
Clear reporting is essential for appropriate clinical decisions and should include1,4:
- Clone size for each cell lineage (ie, granulocytes, monocytes, and RBCs)
- Proportion of Type II and III (percentage of GPI-deficient cells) as well as total RBCs
- Sensitivity level used (0.01% high-sensitivity analysis is ideal)
- All previous flow results in order to monitor clonal expansion
- The International PNH Interest Group recommends routine monitoring every 6 months of patients who have an identified clone5
aDetects PNH cells down to a 0.01% clone size.
Labs should perform PNH HSFC on RBCs and on WBCs using >1 reagent1,4
- Evaluation of RBCs alone may underreport clone size due to hemolysis and the dilution effect of transfusions1,4
- “Routine” CD55- and/or CD59-based approaches are neither accurate nor sensitive below the 1% to 4% clone size2
- Granulocytes give most accurate estimate of PNH clone size2
- FLAER/CD24 or FLAER/CD157 combinations recommended to detect PNH granulocytes2
- Low RBC clone size compared to WBC clone size indicative of intravascular hemolysis1,4
International Clinical Cytometry Society and International PNH Interest Group guidelines
ICCS and IPIG guidelines recommend:
- Testing high-risk patients2,5,6
- Testing patients who meet the criteria within any of the high-risk groups for PNH with high-sensitivity flow cytometry with FLAER on peripheral blood, the standard diagnostic test for PNH1,5,7,8
ICCS guidelines recommend testing patients with:
- Cytopenias and hemolysis or thrombosis or patients with cytopenias that remain unexplained after a thorough workup1
- Unexplained or unprovoked thrombosis or with unexplained cytopenias for PNH
- The risk of thrombosis in PNH is based on terminal complement–mediated attack that leads to the multifactorial prothrombotic risk in PNH1,3,5,9
- Aplastic anemia and myelodysplastic syndrome for PNH with flow cytometry with FLAER performed on peripheral blood1,7
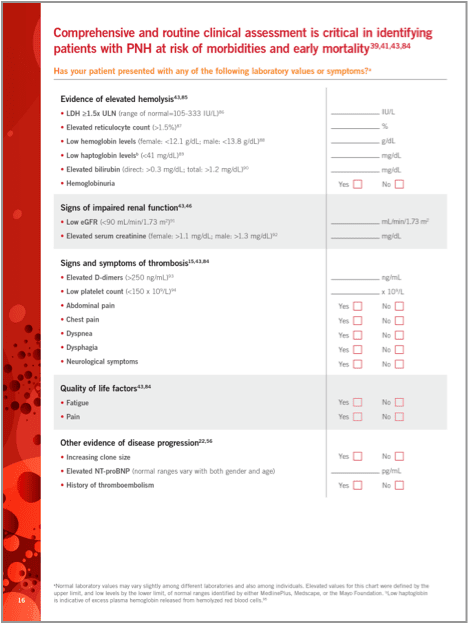
Once positive for PNH, monitor LDH levels
LDH is an important clinical marker of terminal complement–mediated intravascular hemolysis and an important measure of severity of PNH disease activity10-12
LDH ≥1.5 x ULN has been shown to significantly increase the risk for thrombosis and be a predictor of premature mortality in patients with PNH.11,12,b,c
- Patients with PNH and LDH ≥1.5 x ULN had a 4.8-fold higher mortality rate compared with the age- and sex-matched general population (P<0.001).12,b
- LDH ≥1.5 x ULN alone or in combination with chest or abdominal pain has been reported to increase the risk of thrombosis and premature mortality in patients with PNH.11,12,b
Hemolysis as measured by LDH and clinical symptoms are associated with increased risk of thrombosis in patients with PNH11,c

bA retrospective chart review of 301 patients with PNH, enrolled into the South Korean PNH registry, assessed the clinical signs and symptoms predictive of mortality using a standardized mortality ratio compared with an age- and sex-matched general Korean population.12
cA retrospective analysis of 301 patients from the South Korean PNH registry evaluated risk factors for thrombosis using a multivariate analysis matched for age, sex, and bone marrow failure. Data are presented as odds ratios comparing patients with LDH ≥1.5 x ULN with specified symptoms to patients with LDH <1.5 x ULN and no symptoms.11
PNH Resources
ACD=adenosine, citrate, dextrose; EDTA=ethylenediaminetetraacetic acid; FLAER=fluorescent aerolysin; GPI=glycosylphosphatidylinositol; ICCS=International Clinical Cytometry Society; IPIG=International PNH Interest Group; LDH=lactate dehydrogenase; PNH=paroxysmal nocturnal hemoglobinuria; ULN=upper limit of normal.
- Borowitz MJ, et al. Cytometry B Clin Cytom. 2010;78(4):211-230.
- Sutherland DR, et al. Cytometry B Clin Cytom. 2018;94(1):23-48.
- Sharma VR. Clin Adv Hematol Oncol. 2013;11(9)(suppl 13):2-8.
- Illingworth A, et al. Cytometry B Clin Cytom. 2018;94(1):49-66.
- Parker C, et al. Blood. 2005;106(12):3699-3709.
- Sahin F, et al. Am J Blood Res. 2016;6(2):19-27.
- Dezern AE, Borowitz MJ. Cytometry B Clin Cytom. 2018;94(1):16-22.
- Brodsky RA. Hematology: Basic Principles and Practice. 7th ed. Elsevier; 2018:415-424.
- Morado M, et al. Cytometry B Clin Cytom. 2017;92(5):361-370.
- Schrezenmeier H, et al. Haematologica. 2014;99(5):922-929.
- Lee JW, et al. Int J Hematol. 2013;97(6):749-757.
- Jang JH, et al. J Korean Med Sci. 2016;31(2):214-221.